Nursing Home Staffing Shortages and the New Federal Nursing Home Standards
Background
Nursing homes in the U.S have major staffing shortages that can lead to poor quality of care for residents. A 2022 report by the National Academies found that “adequate staffing in nursing homes has been difficult to achieve for multiple reasons, including a negative perception of nursing homes, unsupportive working conditions, and poor pay and benefits.” The COVID-19 pandemic exacerbated these staffing challenges, and effects of the pandemic persist today.
Recognizing that understaffing in U.S. nursing homes has been a concern for many years, the Centers for Medicare & Medicaid Services (CMS) proposed new minimum staffing standards for long-term care facilities. The proposed rule was published for public comment in the Federal Register on September 6, 2023. CMS recently completed reviewing the nearly 47,000 comments and announced details of the final rule on April 23, 2024. The rule requires a daily minimum of 2.45 hours of nurse aide (NA) time per resident (referred to as hours per resident day, or HPRD) and 0.55 daily hours of time by registered nurses (RNs) per resident. The final rule added a requirement for an additional 0.48 HPRD, which can be provided by any combination of nursing staff (RNs, licensed professional nurses, licensed vocational nurses, or NAs).
Increasing staffing to meet these mandated levels at all facilities requires significant growth in nursing staff: In the original draft rule, CMS estimated a need for 12,639 additional RNs and 76,376 NAs nationwide. These requirements are reflected in our previous estimates that, in the fourth quarter of 2022, just half of U.S. nursing homes would have met the new RN standard, while only 28% would have met the NA standard. Average RN and NA staffing levels in this quarter were 0.58 and 2.16 HPRD, respectively. However, there is wide variation among nursing homes around these overall HPRD levels. This has led us to investigate the following question: What characteristics of nursing homes are associated with a higher probability of meeting the newly proposed standards? To address this question, we performed an analysis to examine the association between whether a nursing home meets the standards and the following characteristics of the home:
- Whether the home is in a rural rather than non-rural county (under the hypothesis that homes in rural counties might have relatively greater difficulty in recruiting staff)
- Whether the home is operated by a for-profit rather than nonprofit provider (given the evidence that lower-staffed facilities are more likely to be for-profit)
- The percent of the home comprising residents who are persons of color (to investigate potential equity issues)
- The percent of residents in the home whose primary funding is Medicaid, as opposed to Medicare or private payer funding (Medicaid typically reimburses for care at lower rates than other payers)
We also examined variation among states in the extent to which the above four characteristics affect the percentage of nursing homes meeting the standards.
Data and Methods
Nursing home staffing levels used in this analysis are based on the Payroll-Based Journal (PBJ) Public Use Files for nursing staff, submitted quarterly by nursing homes in the U.S. and published by CMS. These files provide detailed information on staffing each day for every nursing home in the country. Our analysis is based on quarterly summaries of these data prepared by the nonprofit Long Term Care Community Coalition. These publicly available summaries are easier to use than the massive CMS data, and their use has been recommended by other researchers. We analyzed staffing levels during the fourth quarter of 2021, which is the most recent period for which values for the characteristics listed above were available when the analysis was conducted. These data include both employed and contracted staff. We used these staffing levels to compute whether each of the 14,628 nursing homes in the dataset would have met both the RN and the NA standards. Our analysis does not factor in the requirement for the additional 0.48 HPRD that was added in the final rule, as it was added post-analysis. A preliminary analysis of this additional requirement suggests that it has little impact on the results reported here, as noted in the Results section. In assessing whether the RN standard is met, we used the total number of RNs, including administrative as well as direct care staff. The rural vs. non-rural status of each home is based on the National Center for Health Statistics Urban-Rural Classification Scheme for Counties, with county designations taken from the PBJ data. We interpreted counties coded at levels 1 through 4 as non-rural (the levels designated as including metropolitan counties) and levels 5 and 6 as rural (the levels including nonmetropolitan counties).
We extracted the remaining three characteristics from the 2021 LTCFocus dataset and linked them to the PBJ data. This dataset, which lists many characteristics of U.S. nursing homes, excludes data for Alaska (12 facilities) and the District of Columbia (17 facilities), which we have therefore excluded from our analysis. (All 12 nursing homes in Alaska meet the new RN and NA standards; 8 of the 17 homes in the District of Columbia meet the standards.) For an additional 286 facilities, there was no match between the LTCFocus data and the PBJ data; we also omitted these facilities from the analysis.
Values for the percentage of residents who identified as persons of color were computed as 100% minus the percent of residents who identified as White. Values for the percentage of White residents were not reported for 352 facilities because they represented a low number of individuals (fewer than 10). We excluded these facilities from the analysis.
We used a final dataset of 13,961 nursing homes in all the results that follow except those that describe the overall percentages of nursing homes that meet the standards (e.g., Exhibit 3), which include all 14,628 facilities.
We performed a multivariable logistic regression to assess the relationship among these four independent variables (including interactions among them) and the probability that a nursing home would meet the staffing standards. Profit status, percent of residents who identified as a person of color, and percent of residents funded by Medicaid are all highly significant in the regression (p<.001); rural location is not significant. We also conducted state-level analyses to identify the impact of each of the four independent variables on the rate at which nursing homes in each state would meet the standard. Details of all these analyses are in the appendix.
Results
The PBJ data indicate that, in the fourth quarter of 2021, 53% of nursing homes would have met the new RN standard, 28% would have met the new NA standard, and just 20% would have met both standards. Including the recently added 0.48 HPRD requirement has no significant effect on the 20% result: Only 5 fewer nursing homes would have met the standard with the additional 0.48 HPRD requirement than without it. These rates are nearly the same as those found for August 2023 by the Kaiser Family Foundation (KFF) (52%, 27%, and 19%, respectively). In the following two sections, we assess the impact of characteristics of individual nursing homes on their probability of meeting the proposed standards, and the impact of state-level differences in these characteristics on the percentage of homes that would meet the standards.
Impacts on Individual Nursing Homes
We used the regression results (detailed in appendix Exhibit A1) to estimate the marginal effects of each nursing home characteristic, comparing how changes in one characteristic affected the predicted probability of nursing homes meeting the new RN and NA staffing requirements. These marginal effects were developed off a baseline case in which a nursing home was nonprofit, located in a nonrural county, had an average percentage of persons of color (23%), and had an average percentage of residents whose primary payment method was Medicaid (60%). This approach facilitates understanding of the individual impacts of the four independent variables on meeting the staffing requirements.
A nursing home with these baseline characteristics would have a probability of meeting the proposed standards of 0.30 (i.e., 30%). If instead this home were in a rural location, this probability would increase to 33% (rural status was not statistically significant in the regression). If the home were for profit rather than nonprofit, the probability would be reduced from 30% to 11%. This result is reasonably consistent with KFF’s observation that “most (90%) for-profit nursing facilities would need to hire more RNs or nurse aides compared with 60% of government and nonprofit facilities to comply with proposed HPRD staffing minimums.”
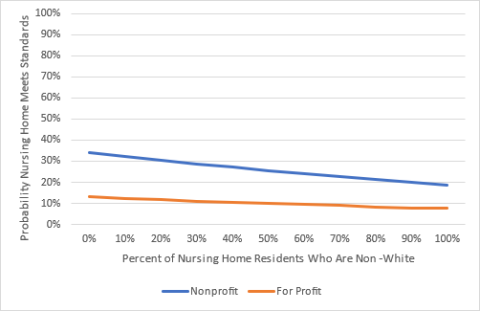
Exhibit 1 illustrates the probability that the standards are met as a function of the percent of the population that identifies as a person of color, showing a decline in the probability as the that population rises. Results are shown for both nonprofit and for-profit centers. Our analyses revealed that nonprofit homes with 50% residents who are persons of color would have a probability of meeting the standards of 26%. This probability is lowered to 19% for homes with 100% persons of color.
Exhibit 1. Impact of Persons of Color Population of Probability of Meeting Standards (Non-Rural County, Average Percent Medicaid)
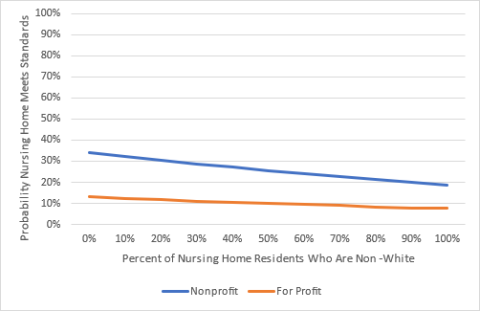
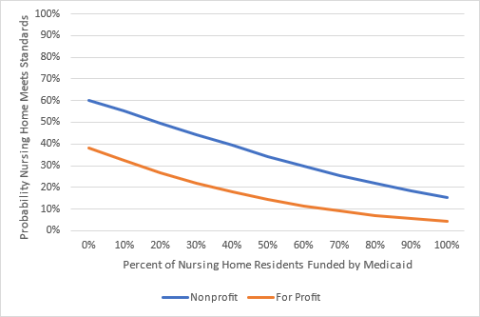
Exhibit 2 provides a similar depiction of the relationship between meeting the proposed standards and the percent of the population whose primary payer is Medicaid, indicating that the probability of meeting the standards decreases with an increase in Medicaid funding. We found that nonprofit homes with 50% of residents who are Medicaid-funded would have a probability of meeting the standards of 34%. Homes with 100% Medicaid-funded residents would have a probability of meeting the standards of 15%.
Exhibit 2. Impact of Medicaid-Funded Population on Probability of Meeting Standards (Non-Rural County, Average Percent Persons of Color)
Impacts on Nursing Homes by State
There is wide variation among states in the percent of nursing homes that meet the new standards. Exhibit 3 displays the percent of homes in each state that already met the new standards in the fourth quarter of 2021, as captured in the PBJ data. Values range from 100% in Alaska to 2.4% in Louisiana, with 32 states falling below the average of 27.2%. The color coding indicates that most states in the West were above the national median, while most in the South were below it.
Exhibit 3. Percent of Nursing Homes Meeting the New Staffing Standards, Fourth Quarter of 2021
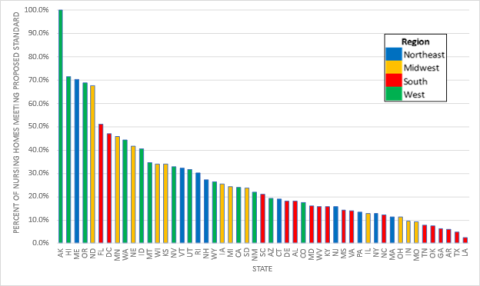
KFF notes that “variation across the states is likely to reflect many factors, including what percentage of facilities are for-profit, the availability of RNs and nurse aides in the state, and state requirements regarding minimum staffing levels.”
To explore the hypothesis that state requirements affect the variation across states, we examined existing staffing standards for RNs plus NAs that have been established within each state, using data from the State Nursing Home Staffing Standards Chart compiled by Consumer Voice. We found no relationship between these state-level standards and the percent of nursing homes in the state that would have met the combined proposed federal standard (r=-0.06). However, most state standards are well below the new federal standards (averaging 1.6 HPRD), with only 7 states having standards that exceed the federal ones. In a detailed analysis of Massachusetts’ new standard of 3.58 HPRD, Abt Associates concluded that the new standard did result in statistically significant, though small, increases in staffing levels.
Instead, we focused on the impact of the same four independent variables (location, ownership status, percent of persons of color, and percent on Medicaid) on the rates at which the federal standards were met in each state in the fourth quarter of 2021:
- Rural vs. non-rural location. In 9 states, facilities in rural counties had a significantly different rate of meeting the standards than those in non-rural counties (p<.05). Of these nine, four were actually more likely to meet the standards when in rural counties. These mixed results for a small number of states are consistent with our national regression results, for which rural status was not significantly associated with the probability the standards were met.
- Nonprofit vs. for-profit status. In 39 states, facilities with nonprofit status had a significantly higher rate of meeting the standards than those that are for-profit (p<.05). Ignoring significance, all but one state showed a higher percentage of meeting the standards for nonprofit homes (and the result for that one state with a lower percentage was not significant).
- Percent of residents who are persons of color. To investigate the impact on state-level results of racial mix, we conducted a logistic regression to determine the impact of the percent of residents of color in facilities within each state on the probability of meeting the standards. In 22 states, the percentage of residents who are persons of color in a facility had a significant impact on the rate of meeting the standards (p<.05). All 22 had a decreasing probability of meeting the standards with an increase in percent of residents of color.
- Percent of residents on Medicaid. To investigate the impact of Medicaid funding on state-level results, we conducted a logistic regression to determine the impact of the percent of Medicaid-funded residents in facilities within each state on the probability of meeting the standards. In 34 states, the effect was significant (p<.05). In all of these 34, increased Medicaid coverage was associated with a decreasing probability of meeting the standards.
Details of these results for individual states can be found in the appendix.
Discussion
We have examined the relationship between four independent variables—location, ownership status, percent of persons of color, and percent on Medicaid—and the probability that a nursing home meets the new HPRD staffing standards. Because our analysis controls for other factors while examining the impact of a single characteristic, we are able to better understand the impact of each factor on staffing levels. We have shown that ownership status (for-profit vs. nonprofit) is strongly related to the probability that a nursing home meets the new staffing levels, with nonprofit homes significantly more likely to meet the standards. This observation is consistent with results described by other researchers. We also found that a higher percentage of residents covered by Medicaid is associated with a lower probability that the proposed standards are met. This finding is not surprising given Medicaid reimbursement rates for nursing home stays are lower than from Medicare or private payers, and because the intensity of care needed by Medicaid residents tends to be lower than for those funded by Medicare or private payers. We found a negative relationship between the percentage of a nursing home’s population that identifies as a person of color and its probability of meeting the staffing standards, suggesting a significant health inequity in the quality of nursing home care received by residents who are persons of color. Finally, the rural vs. non-rural location of nursing homes did not show an impact on the probability of meeting the standards, suggesting that location might not significantly affect facilities’ ability to recruit staff from less-populated areas.
The similarity of our results to those of other researchers who addressed some of the same questions using more recent data suggests that our use of older PBJ data is unlikely to have had a substantial impact on these observations.
Our state-level analyses highlight the large differences in the extent to which nursing homes in different states meet the new federal standards. Whether a nursing home had a rural vs. non-rural location did not show to be a significant predictor of meeting the standards in most states, and the results are mixed for the few states in which it is significant (nursing homes in four of nine states were more likely to meet the standards when in rural counties). In contrast, ownership status has a significant impact on meeting the standards in most states. Our analysis showed a lower percentage of homes that are for-profit meet the standards than nonprofit homes. In nearly half of the states, homes with a relatively high percentage of residents of color are less likely to meet the standards than those with no or few persons of color, suggesting that the health inequities identified at the national level may be present in a number of states. Finally, homes in two-thirds of the states have a significantly lower probability of meeting the standards with increasing numbers of residents who are financed by Medicaid.
As we have noted previously, current staffing levels in nursing homes are likely inadequate to provide safe, high-quality care for residents. Achieving the new federal staffing standards will require a significant increase in the numbers of RNs and NAs employed by nursing homes and would be expected to increase the total costs required for nursing homes across the country, both through the need to pay additional staff and the higher wages that will likely be needed to attract them. CMS estimates that the economic impact of the staggered implementation of the staffing-related provisions of the rule will total $43 billion for the first 10 years. These increased costs will likely cause increases in spending on nursing home care to account for these changes. Our most recent Health Sector Economic Indicators (HSEI) spending data show that nursing home spending increased by nearly 11% year-over-year in 2023 and was nearly 27% higher in February 2024 than it was in December 2019 (before the start of the pandemic). Increasing staffing levels to meet the new requirements will require similar overall spending growth rates. To the contrary, if such standards were not enacted with the resources required to meet them, the extensive understaffing described in this paper would likely continue. The relationships identified here might help focus policy initiatives aimed at meeting the new standards.
See materials below for appendix and references.