
The Health Care Workforce Crisis Arrives at the PACE Model
While employment in the health care sector has largely rebounded following the Covid-19 recession, health care employers (especially in long-term care) continue to struggle with recruiting and retaining workers. A recent American Health Care Association survey of nursing homes found that 87 percent were experiencing moderate or severe staffing shortages, and employment in residential care overall remains below pre-pandemic levels. Similarly, a recent Kaiser Family Foundation study of state Medicaid programs revealed a shortage of home and community-based services workers in 45 states.
According to the second and final Altarum Program of All-Inclusive Care for the Elderly (PACE) Pandemic Response Survey, PACE organizations across the country have not been spared from workforce challenges, which threaten to complicate service delivery for PACE participants. Similar to other health care employers, PACE centers have responded with various strategies to stabilize their workforces and mitigate the effects of workforce shortages, but the long-term impact of these efforts remains largely unknown.
Altarum fielded our most recent PACE Pandemic Response Survey from May to September 2022 as part of our comprehensive study on the PACE model during the Covid-19 pandemic. Previously in 2021, we administered the first PACE Pandemic Response Survey to PACE directors and heard qualitative reports of their remarkable adaptations to deliver care safely during the public health crisis. However, ensuring participant safety was not their only challenge; PACE directors also reported their acute workforce shortages. Our second survey aimed to quantify and deepen our understanding of the reported themes. Ninety-two PACE directors responded to the most recent survey, representing about three-quarters of PACE sites nationwide.
PACE Sites Are Struggling to Recruit and Retain Workers
Nearly all PACE directors (97 percent) said they were experiencing a workforce shortage. This figure includes 92 percent who reported difficulty filling open positions and 51 percent with higher-than-usual turnover. The positions most likely to be open were home-based personal care staff, nurses, drivers, and center-based personal care staff. Nearly all PACE directors were concerned about filling their openings. And more than half of PACE directors hiring for nurses and personal care staff were “extremely concerned” about filling these positions. (See Figure 1.)
Figure 1: PACE Site Hiring Needs and Level of Concern About Filling Openings by Occupation

Like other health care providers, PACE sites face exceptionally tight competition for workers in the current labor market. Nurses are in extremely high demand across health care sectors and many providers have started offering higher wages, large bonuses, flexible scheduling, and other incentives to attract and retain them. Also, jobseekers who could fill PACE openings with lower entry-level requirements (e.g., for personal care and transportation roles) have numerous high-paying, perk-laden employment opportunities to choose from in industries like retail, food service, and fulfillment centers. These job prospects may also entice current PACE workers to leave their jobs, leading to higher turnover.
However, PACE sites have recruitment and retention advantages over other health care employers. Research and reports from the field indicate that personal care staff in PACE sites have higher job satisfaction, a greater sense of teamwork, and feel more valued for their opinions than direct care workers in other settings. This is likely because PACE personal care staff, and a variety of other health care and social service staff, work together in interdisciplinary care teams—a signature feature of the PACE model.
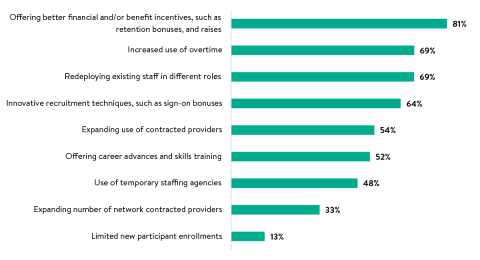
Also, unlike other health care employers, PACE centers have flexibility in spending their Medicare and Medicaid-funded capitated reimbursement rates, allowing them to invest in recruitment, retention, and shortage mitigation strategies. For example, 81 percent of PACE directors reported they invested in wage raises, benefits, retention bonuses, and other financial incentives, and 69 percent relied more heavily on staff overtime. (See Figure 2.) Many PACE sites also extensively used contracted providers and temporary staffing agencies. They also made up for staffing shortfalls with operational changes, like redeploying existing staff (69 percent). All these investments and innovations helped PACE sites to continue enrolling new participants; just 13 percent of PACE sites limited the number of new participant enrollments due to limited staff capacity caused by shortages.
Figure 2: PACE Organization Strategies to Address Workforce Shortages
Effects of Workforce Shortages on PACE Services
While most PACE sites stayed open to new participants, they still likely faced extensive operational challenges due to staffing shortages. First, staff shortages could hinder PACE sites’ capacity to sustain the numerous and creative adaptations they employed during the Covid-19 pandemic because many of these adaptations required additional staff time. Nearly every PACE director (96 percent) said they increased in-home personal care services for PACE participants during the pandemic, and 70 percent implemented and planned to continue these services. However, as noted above, PACE directors reported the most difficulties filling in-home personal care worker positions.
Beyond adaptations, shortages could impact PACE services in other ways. Short staffing among nurses and direct care staff could mean these workers have less time to spend with participants, and fewer drivers could pose barriers to community inclusion and health care access for PACE participants. Also, unfilled positions could lead to knowledge gaps in interdisciplinary care teams.
These survey findings are all critical context for the final phase of our PACE pandemic response research—a comparison of care outcomes for PACE participants and Medicare fee-for-service beneficiaries during the height of the COVID-19 pandemic. We will release those findings later this year.
In sum, despite their current challenges, PACE programs are well-positioned to stabilize their workforce and continue delivering high-quality care. The Altarum PACE Pandemic Response Survey results have demonstrated the remarkable ways PACE programs adapted services for participants during the Covid-19 pandemic, and the diversity of strategies they have already adopted to address workforce shortages. That flexibility and innovative thinking will be necessary to weather the national health care workforce crisis.
Experts
